By Sudarshan Pyakurel MA MSW LSW

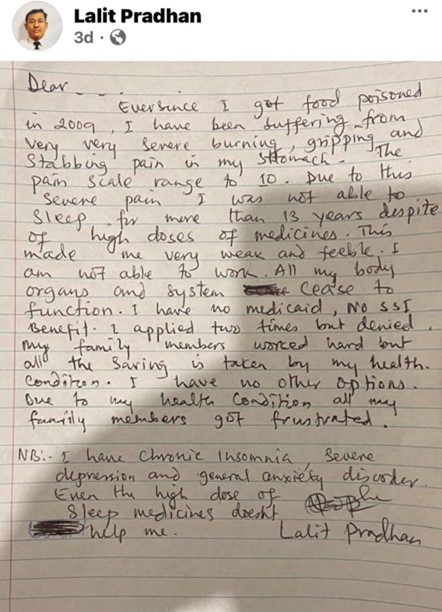
The recent case of Lalit Pradhan, whose suicide note was followed by a tragic homicide–suicide has sparked an online debate, especially on social media. First, this is an unfortunate and devastating loss. The family members are victims of this incident, and the entire community, particularly Bhutanese -Nepali families, is deeply shaken.
We must recognize that many of us carry the invisible burden of untreated mental illness, often rooted in refugee experiences, historical trauma, persecution, and social isolation. While some have been able to heal and move forward due to changed circumstances, not everyone’s journey is the same.
Mental well-being is shaped by a complex interplay of factors like genetics, past trauma, social environment, economic stress, and even untreated physical illnesses, which can lead to or worsen mental health conditions over time (World Health Organization, 2022). What we should not expect from someone with a severe mental illness is rational decision-making that aligns neatly with societal norms.
Some online commentators have expressed disgust or moral outrage at the nature of the tragedy. But this misunderstanding is part of the problem. Severe mental illness can fundamentally impair judgment, distort perception, and alter one’s sense of morality. Not because the person “chooses” to be this way, but because the illness itself changes how the brain processes reality (American Psychiatric Association, 2022).
In advanced stages of mental illness, the mind, body, and spirit – the three interconnected aspects of a person’s whole health can become unsynchronized. This “disconnection” manifests in personality changes, unpredictable behavior, and altered moral reasoning. In these moments, the person is not consciously making harmful decisions; rather, events happen “through them,” as the illness takes over essential cognitive and emotional functions.
People with severe mental illness may see or hear things that others cannot (hallucinations), or hold deeply fixed beliefs that are out of touch with reality (delusions). These experiences are not “made up” or simply wild imagination. For the person, they are a genuine and unshakable reality, just as our shared reality feels unshakable to us.
For those of us considered “mentally healthy,” reality is something we collectively agree upon. It is a consensus with no perceived alternative. For someone in the grip of severe mental illness, their altered reality is equally non-negotiable. This is why empathy and understanding are critical; the difference between their reality and ours is not a matter of choice, but of neurological and psychological changes beyond their control.
Importantly, episodes of altered reality are not exclusive to psychiatric diagnoses. Many of us have experienced brief distortions in perception or thought during times of extreme stress, sleep deprivation, or severe physical illness. In that sense, mental illness is not a distant or alien phenomenon. It is a condition closer to all of us than we might like to believe.
When Everyday Glitches Mirror Severe Mental Illness
Most of us have experienced brief lapses in decision-making like stopping at a green light for a few seconds before realizing it was a go, not a stop or starting to cross a street during the “Don’t Walk” signal and suddenly changing direction mid-way or freezing in place when a quick decision is needed. These seemingly small “glitches of the mind” can sometimes lead to accidents or near misses.
Such lapses are often linked to stress, medication side effects, fatigue, or recent life changes. Now, imagine a person who has lived for years or decades under high stress, chronic pain, insomnia, and perhaps the lingering effects of trauma. Research shows that in the United States, the average time from the onset of mental illness symptoms to receiving appropriate treatment can range from 8 to 11 years (National Alliance on Mental Illness, 2023). Over such a long period, a person’s ability to make even the simplest decisions like recognizing that a green light means “go” can be impaired many times over.
Yet life demands far more than just simple traffic decisions. It requires navigating complex choices that are shaped by cultural norms, social expectations, laws, and relationships. This is why, in legal systems around the world, when a person commits a crime under the influence of a severe mental health condition, there are provisions. Such as the insanity defense that recognizes they may not be fully responsible for their actions. The illness, not the individual’s moral compass, is often at the root of the behavior (American Bar Association, 2020).
As a society, we must be willing to apply the same principle of compassion and medical understanding to tragedies like the Lalit Pradhan case. This is not about excusing the act or minimizing the harm caused. It is about recognizing that severe mental illness can strip away the capacity for rational choice. Factors such as gender, wealth, ethnicity, or immigration status may influence the development or progression of mental illness, but the ultimate act often lies beyond the reach of ordinary social expectations, and in some cases, beyond the grasp of the legal system’s standard accountability framework.
This is not a defense of Lalit Pradhan or anyone in similar circumstances. Rather, it is an attempt to challenge the prevailing notion that such acts are purely “individual choices” rooted in ego or desperation. Just as death from cancer is not a “choice” but the result of a disease process that the body could not overcome, a violent or self-destructive act in the context of severe mental illness must be seen through a similar medical lens.
One common analogy in mental health education is the conversation between two friends. One with asthma (A) and one without (B). B says: “There’s so much fresh air outside, why can’t you just breathe normally?” A replies: “It’s not the air that’s the problem, it’s my lungs.” Similarly, mental illness is not simply about external circumstances or a lack of willpower, but about internal neurobiological changes that alter perception, judgment, and behavior.
Genetics, Resilience, and the Cultural Gap in Mental Health Care
Some may argue: “I’ve faced similar hardships. I was a refugee too. I lost my family in the conflict. I was imprisoned, I went through divorce, or I grew up with a single parent, and yet I didn’t commit such an act.” Yes, adverse life experiences can contribute to mental illness. But what often gets overlooked is the underlying neurobiological vulnerability, sometimes referred to as a genetic predisposition.
In simple terms, some people’s brains are “hard-wired” to recover more quickly from trauma. This is the resilience factor. Others, however, lack this protective wiring at the genetic or neurochemical level. When the “right” combination of stressors appears like prolonged loss, chronic stress, untreated illness, it can trigger lasting neurochemical changes in the brain. These changes can become the person’s “new normal,” even though they may no longer fit the demands, norms, and expectations of the surrounding society.
Consider someone who has battled insomnia, depression, or anxiety for years. Over time, their brain chemistry and neural pathways may shift permanently, not irreversibly, but requiring targeted, specialized interventions. For first-generation immigrants in the United States, these interventions are often inaccessible due to language barriers, cultural taboos, societal stigma, financial hardship, and the dominance of Western-centric treatment models that may not align with their cultural values.
As a result, some individuals with severe mental illness may resort to extreme actions like harming themselves or loved ones. Not because they believe it’s the “solution,” but because their altered mental state drives behaviors outside of conscious control. There is no fixed “pattern” to these tragedies, which makes research and prevention extremely difficult.
Researchers are often left with fragmented data and no clear way to connect the dots. This is why we urgently need community-led, culturally grounded research that informs the development of culturally appropriate interventions. Mental health services for immigrant and refugee communities must involve family members in the treatment and healing process, because without community and family integration, recovery is vastly harder. Even when help is available, it is often not well-informed or culturally attuned.
It is important to remember mental illness is not just about “chemical imbalance” in the brain. It is also shaped by the epigenetic environment, the interaction between our genes and lived experiences, and by the broader societal systems in which we live. There is no “one-size-fits-all” approach to diagnosis, treatment, or recovery. Addressing mental illness, particularly in refugee and immigrant populations, requires a society-wide commitment to changing the social, economic, and political conditions that either support or undermine mental well-being.
References:
● Alegría, M., Álvarez, K., & DiMarzio, K. (2017). Immigration and mental health. Current Epidemiology Reports, 4(2), 145–155. https://doi.org/10.1007/s40471-017-0111-2
● American Bar Association. (2020). Insanity defense in the United States. https://www.americanbar.org/groups/public_education/publications/insights_on_law_andsociety/19-1/insanity-defense-in-the-united-states/
● American Psychiatric Association. (2022). Understanding Mental Disorders: Your Guide to DSM-5-TR. American Psychiatric Publishing.
● National Institute of Mental Health. (2023). Genes and mental illness. https://www.nimh.nih.gov/health/publications/
● National Alliance on Mental Illness. (2023). Mental health by the numbers. https://www.nami.org/mhstats
● World Health Organization. (2022). World Mental Health Report: Transforming mental health for all. https://www.who.int/publications/i/item/9789240063600
Support the New Americans magazine to continue to serve our community with precise news that affect the new American, immigrant and refugee community. https://paypal.com/donate/?hosted_button_id=8LHFS78NRNJJY&source=url






































Leave a Reply
You must be logged in to post a comment.